PCOS and IVF Success Rates
Medically reviewed by Linda Streety, RN, BSN
Polycystic ovary syndrome (PCOS) is common, affecting 1 in 10 people with ovaries. It’s also a common cause of infertility, since up to 80% of people with PCOS experience infertility (1). However, there are many treatments available to patients with PCOS-related infertility.
What is PCOS?
PCOS is caused by an imbalance of reproductive hormones that may correlate with fertility issues and other health problems, such as diabetes, gestational diabetes, and heart disease. PCOS got its name because ovaries appear to have many small cysts when seen by ultrasound. While researchers aren’t sure what causes PCOS, they know that people with PCOS often have insulin resistance (in which the body produces insulin but doesn’t use it well) and high levels of androgens (hormones that can prevent the ovaries from ovulating each menstrual cycle).
How does PCOS affect fertility?
PCOS can affect ovulation because hormone imbalances may lead to follicles that don’t mature enough to release an egg each menstrual cycle. PCOS is also related to insulin resistance, a high BMI, and metabolic syndrome, which are associated with issues with egg quality, embryo quality, uterine lining abnormalities, placenta development, and overall pregnancy outcomes (2).
This may sound discouraging, but PCOS is very often a treatable cause of infertility, and the treatments available are highly effective compared to other infertility diagnoses.
Some of the treatments that people with PCOS can try include:
Lifestyle changes
For people with PCOS with a BMI between 25-27, a modest weight loss of 5% could improve ovulation and pregnancy rates (3).
Medications to restart ovulation
Your clinician may try several medications to help encourage ovulation. These include metformin (a type 2 diabetes drug that can help stabilize the metabolic side of PCOS), and clomiphene or letrozole (to induce ovulation). However, some of these medications come with caveats. Clomiphene is more likely to result in a pregnancy with multiples (twins or triplets), and metformin increases the rate of ovulation but does not necessarily increase the rate of pregnancy (4).
Gonadotropin medications
For patients who don’t respond well to the medications above, low-dose gonadotropin medications can be used to induce ovulation. One study found that 50% of PCOS patients with this type of medication therapy conceived after 6 cycles (5).
In vitro fertilization (IVF)
IVF is an effective treatment for PCOS-related infertility, especially for patients with a good ovarian reserve, and/or patients who are not ovulating.
Patients with PCOS are among the most successful with IVF. Below, you can see the comparison in IVF outcomes for patients with PCOS vs. other infertility diagnoses, according to data pulled from the Society for Assisted Reproductive Technology (SART) between 2014 and 2019. Please note that if a patient experienced two or more infertility diagnoses (for example, male factor infertility and PCOS), they are included in the percentage of success for both diagnoses. Also, these percentages are for all patients on any cycle of IVF.
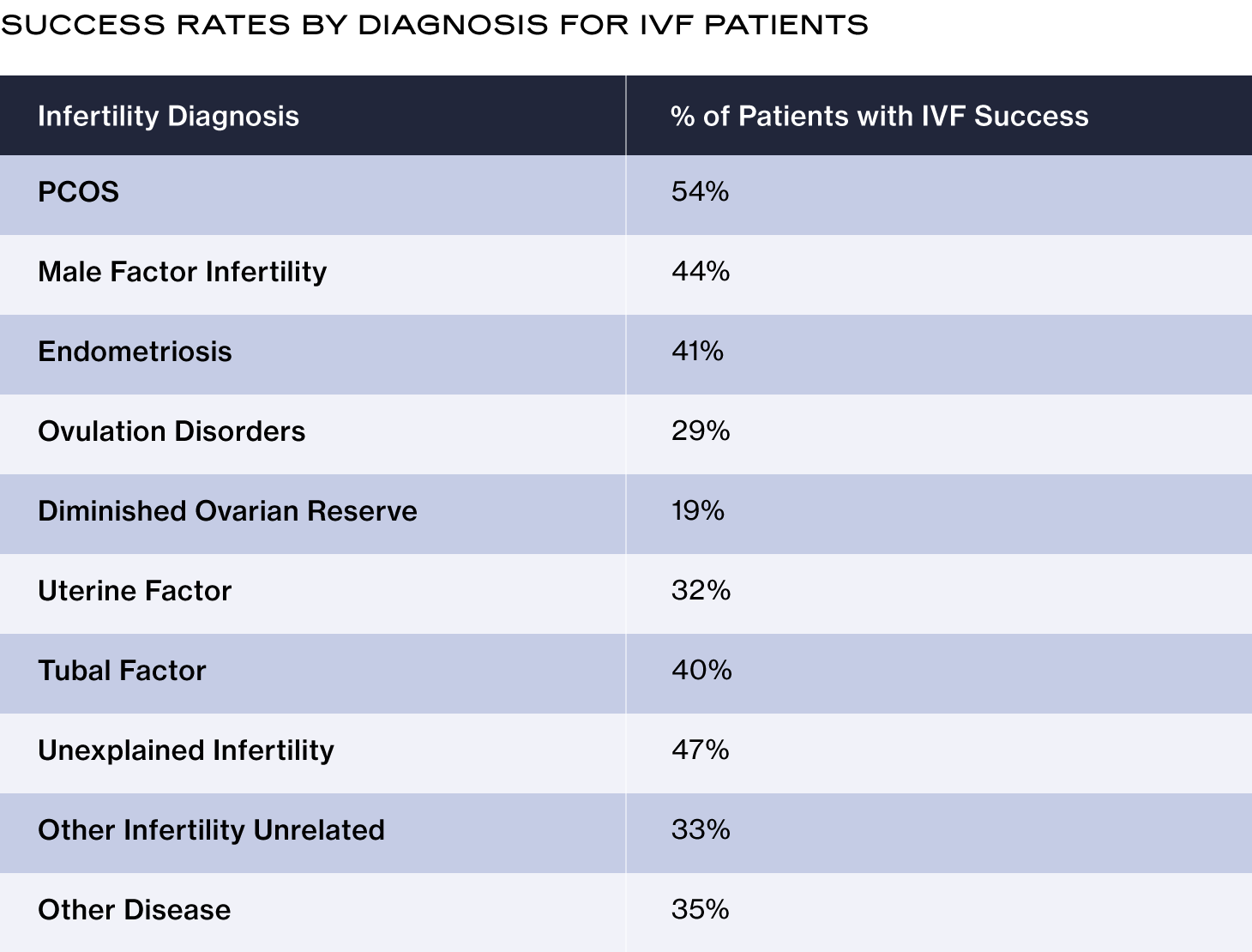
PCOS and IVF success rates
When compared to patients without PCOS, one study found some notable differences in IVF outcomes for patients with PCOS (6). When compared, patients with PCOS experienced:
-
Higher chance of cycle cancellation after starting an ovarian stimulation due to the risk of ovarian hyperstimulation syndrome (OHSS), described in detail in the next section.
-
Significantly more eggs retrieved than other patients.
-
About the same rate of fertilization.
-
No significant difference in clinical pregnancy rate per started cycle.
Most importantly, the study found that overall, patients with PCOS had similar pregnancy and live birth rates as patients without PCOS. In other words, IVF for PCOS results in fairly normal success rates.
Risks of IVF with PCOS and how to prevent them
OHSS
One risk of undergoing IVF with PCOS is the possibility of developing severe ovarian hyperstimulation syndrome (OHSS). OHSS is an uncomfortable and potentially dangerous condition that may occur after egg retrieval if you developed a large number of follicles (more than 20) and/or had high estrogen levels at the end of your ovarian stimulation cycle. During OHSS, fluid builds up in the abdominal cavity. Symptoms that result include bloating, constipation, reduced urinary output, and abdominal pain. More severe symptoms may include rapid weight gain (more than 2.2 pounds in one day), nausea and/or vomiting, severe abdominal pain, and/or shortness of breath.
Patients with PCOS are more likely to develop severe OHSS (15.4%) than patients with normal ovaries (2.7%) (7). If your reproductive endocrinologist (RE) suspects that you are at risk of developing OHSS, they will likely suggest that you use a low-dose GnRH antagonist ovarian stimulation protocol with a GnRH trigger shot (8). (Click here to learn more about ovarian stimulation protocols.) Your RE will likely also recommend a frozen embryo transfer since the risk of OHSS is much higher after a fresh embryo transfer for patients with PCOS.
Early pregnancy loss
Patients with PCOS have a higher risk of early pregnancy loss (30-50%) after IVF than patients without an infertility diagnosis (10-15%) (9). To reduce this risk, your clinician may prescribe metformin, which reduced this risk to 8.8% in one study (10).
Ectopic pregnancy
Patients with PCOS are a higher risk of an ectopic pregnancy if they do a fresh embryo transfer after ovarian stimulation during IVF (11). However, this risk disappeared when patients underwent a frozen embryo transfer. Because of this, your clinician may recommend that you do a frozen embryo transfer to reduce this risk.
Though PCOS can make it difficult to get pregnant without fertility treatment, PCOS is a highly treatable form of infertility and many patients go on to have a successful pregnancy. If you have PCOS, you can work with your clinician to design the best treatment for you.
Recent Articles
References
-
Melo, A., Ferriani, R., & Navarro, P. (2015). Treatment of infertility in women with polycystic ovary syndrome: approach to clinical practice. Clinics, 70(11), 765–769. https://doi.org/10.6061/clinics/2015(11)09
-
Palomba, S. (2021). Is fertility reduced in ovulatory women with polycystic ovary syndrome? An opinion paper. Human Reproduction, 36(9), 2421–2428. https://doi.org/10.1093/humrep/deab181
-
Badawy, A., & Elnashar, A. (2011). Treatment options for polycystic ovary syndrome. International Journal of Women’s Health, 3, 25. https://doi.org/10.2147/ijwh.s11304
-
Treatments for Infertility Resulting from PCOS. (n.d.). Https://Www.nichd.nih.gov/. https://www.nichd.nih.gov/health/topics/pcos/conditioninfo/treatments/infertility
-
Gorry, A., White, D. M., & Franks, S. (2006). Infertility in Polycystic Ovary Syndrome: Focus on Low-Dose Gonadotropin Treatment. Endocrine, 30(1), 27–34. https://doi.org/10.1385/endo:30:1:27
-
Heijnen, E. M. E. W., Eijkemans, M. J. C., Hughes, E. G., Laven, J. S. E., Macklon, N. S., & Fauser, B. C. J. M. (2005). A meta-analysis of outcomes of conventional IVF in women with polycystic ovary syndrome. Human Reproduction Update, 12(1), 13–21. https://doi.org/10.1093/humupd/dmi036
-
Swanton, A., Storey, L., McVeigh, E., & Child, T. (2010). IVF outcome in women with PCOS, PCO and normal ovarian morphology. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 149(1), 68–71. https://doi.org/10.1016/j.ejogrb.2009.11.017
-
Thakre, N., & Homburg, R. (2019). A review of IVF in PCOS patients at risk of ovarian hyperstimulation syndrome. Expert Review of Endocrinology & Metabolism, 14(5), 315–319. https://doi.org/10.1080/17446651.2019.1631797
-
Tandulwadkar, S., Lodha, P., & Mangeshikar, N. (2014). Obstetric complications in women with IVF conceived pregnancies and polycystic ovarian syndrome. Journal of Human Reproductive Sciences, 7(1), 13. https://doi.org/10.4103/0974-1208.130802
-
Jakubowicz, D. J., Iuorno, M. J., Jakubowicz, S., Roberts, K. A., & Nestler, J. E. (2002). Effects of Metformin on Early Pregnancy Loss in the Polycystic Ovary Syndrome. The Journal of Clinical Endocrinology & Metabolism, 87(2), 524–529. https://doi.org/10.1210/jcem.87.2.8207
-
Wang, J., Wei, Y., Diao, F., Cui, Y., Mao, Y., Wang, W., & Liu, J. (2013). The association between polycystic ovary syndrome and ectopic pregnancy after in vitro fertilization and embryo transfer. American Journal of Obstetrics and Gynecology, 209(2), 139.e1–139.e9. https://doi.org/10.1016/j.ajog.2013.05.007
Share this
Recent Articles
Learn everything you need to know about IVF
Join the newsletter for IVF education, updates on new research, and early access to Alife products.



