IVF Follicle Sizes and Growth Chart
Medically reviewed by Linda Streety, RN, BSN
During the ovarian stimulation phase of IVF, your reproductive endocrinologist (RE) looks for consistent growth across your follicles, about 1.7 mm per day. When your RE determines that several of your lead follicles have reached an ideal size, ~ 16-22mm in diameter, they will schedule the egg retrieval procedure.
What exactly are follicles?
Follicles are tiny, fluid-filled sacs in your ovaries, each of which contains an immature egg (sometimes referred to as an “oocyte”). Most of these follicles are in a resting phase at any given time. However, large groups of them are continually “recruited” to grow together, moving through stages of development in a process that takes about a year. During this time, many of the follicles in the group die off. This process, called “atresia,” is totally normal and okay; you want only the strongest follicles and eggs to win out.
About 6-20 of a given group of follicles will reach the later stages of maturity. At this point, these “antral” follicles are large enough to be seen on an ultrasound, since they are each about 2-10mm in diameter.
Ordinarily, your body will select a single dominant follicle to develop fully and mature before the egg is released, or “ovulated.” However, during the ovarian stimulation portion of IVF, you’ll take hormone medications to help you develop much more of this group of follicles to maturity.
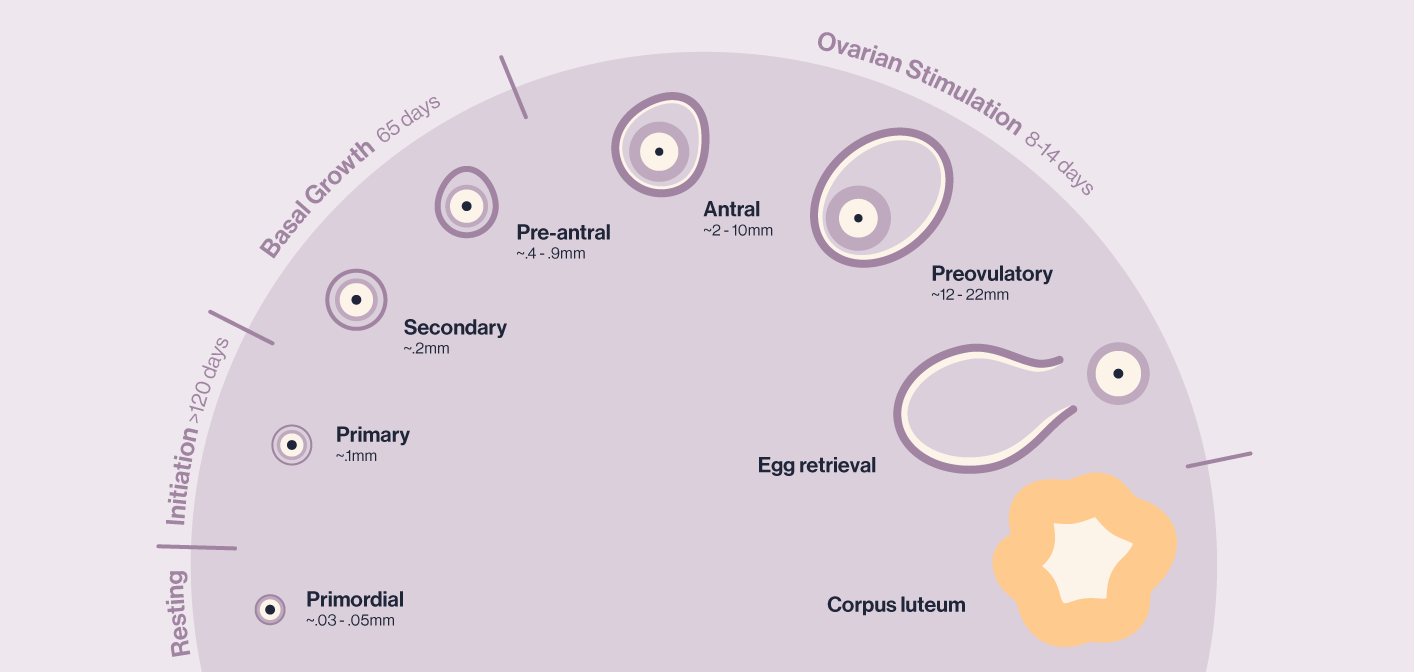
After ovulation during a regular menstrual cycle, the burst follicle becomes a completely normal cyst called the “corpus luteum.” This cyst produces estrogen and progesterone to support an early pregnancy. If no pregnancy occurs, the corpus luteum stops producing hormones after about 12-14 days, and menstruation begins.
During an IVF pregnancy attempt, the medications used during ovarian stimulation disrupt the usual development and function of a corpus luteum (1). Additionally, some of the cells that would go on to produce progesterone are removed along with the egg during the egg retrieval process. As a result, if you underwent ovarian stimulation and plan to undergo a fresh embryo transfer (in which the embryo is transferred 3-5 days after egg retrieval) you will need progesterone supplementation to help support implantation and an early pregnancy. Progesterone supplementation may also be necessary during a frozen embryo transfer, depending on whether you are producing enough progesterone on your own.
Why does follicle growth during IVF matter?
Follicle growth during your IVF cycle must be carefully controlled to ensure that your follicles mature at roughly the same time. This is because the trigger shot administered at the end of ovarian stimulation “triggers” all the available follicles to mature so they can be collected during your egg retrieval. Follicles that are too small and house eggs that aren’t yet mature will generally not be usable during IVF.
What is the ideal follicle growth during IVF?
During ovarian stimulation, your RE will carefully monitor your follicles via ultrasound. They are looking for steady growth that’s consistent across your follicles, about 1.7 mm per day (2). However, they are not just looking at your follicles, they are also monitoring your hormone levels to ensure that you are not at risk of ovarian hyperstimulation syndrome (OHSS). OHSS is an uncomfortable and potentially dangerous condition that may occur if you developed a large number of follicles (more than 20) and/or had high estrogen levels before the egg retrieval procedure.
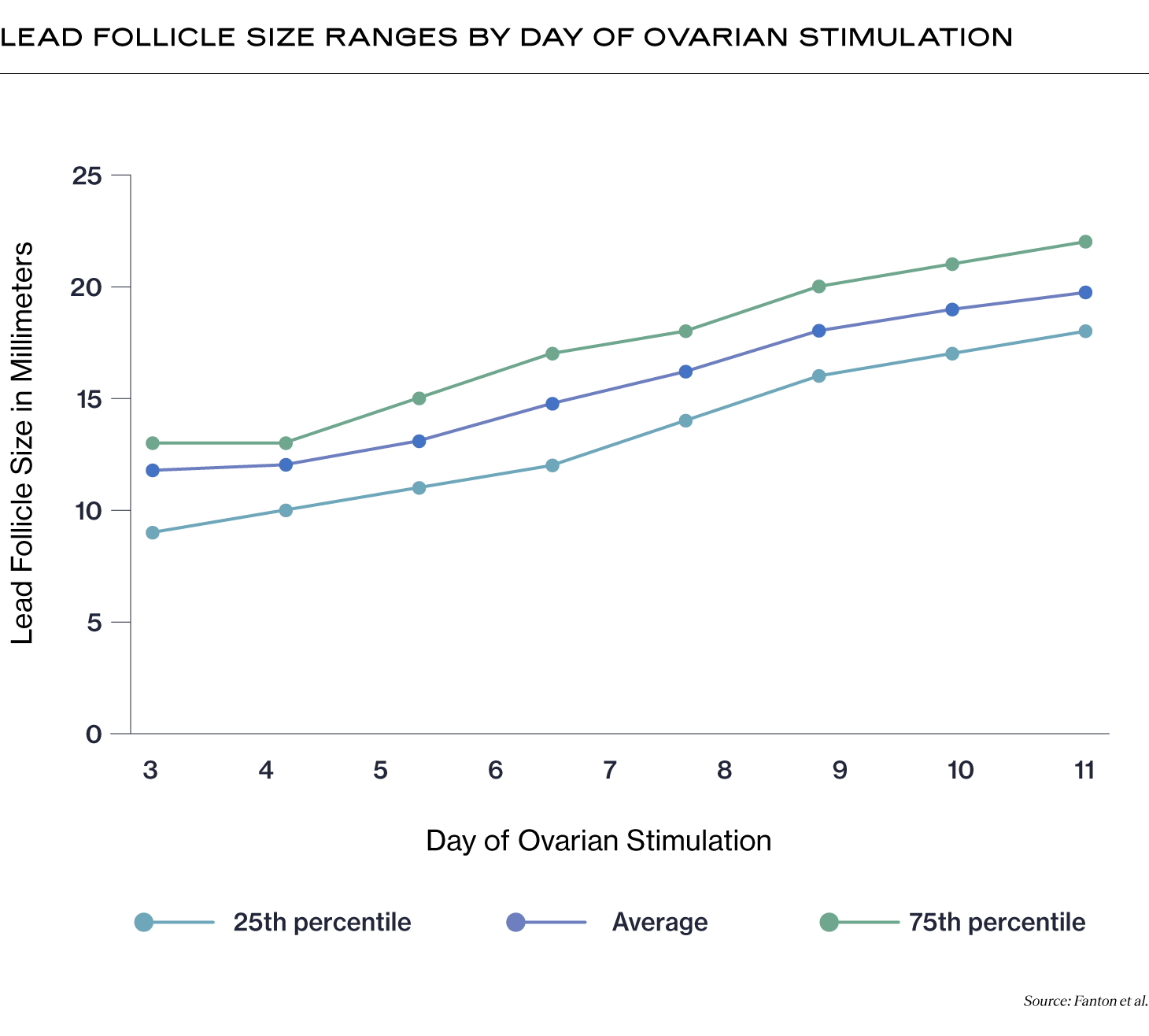
Your RE will be particularly interested in your “lead” follicles. These are the largest follicles out of the group of follicles that are growing together, and tend to contain the eggs that have the best chance of fertilization and becoming a high-quality embryo (3). When your RE determines that several of your lead follicles have reached an ideal size, usually between 16-22mm in diameter, your RE will order a trigger shot and schedule the egg retrieval procedure.
In the IVF follicle growth chart below, you can see a range of lead follicle sizes by day of ovarian stimulation from day 3-11. In addition to the average IVF follicle growth size by day, we included the 25th and 75th percentile follicle sizes so you can see the range of sizes possible.
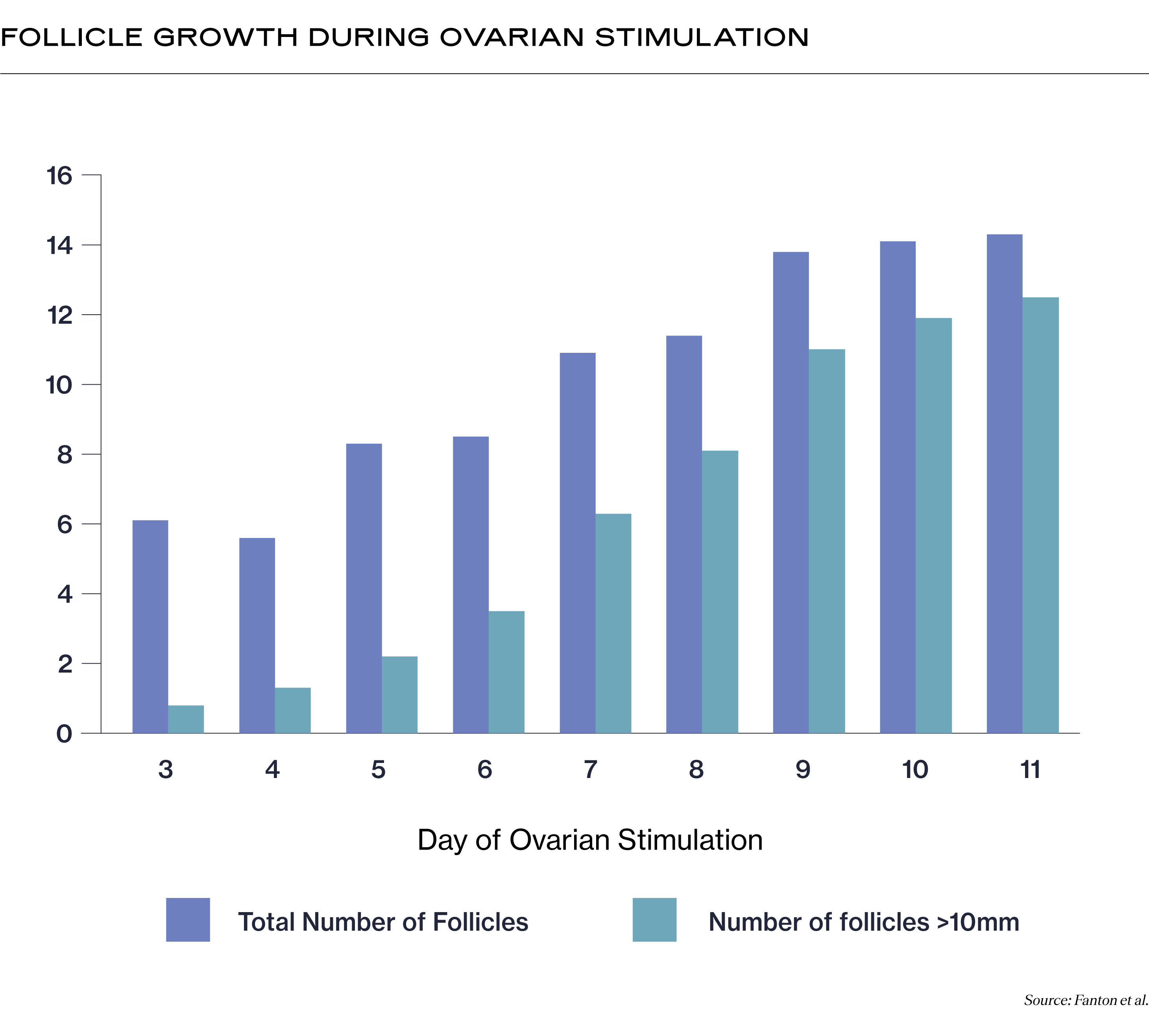
Your RE will also be interested in the number of follicles above 10mm in diameter. This is because follicles that are smaller than that most likely will not contain a mature egg capable of fertilization. So while you may have many follicles that appear on the ultrasound on day 3 of ovarian stimulation, only 1, on average, is above 10mm. But by day 11, most of those follicles are above 10mm!
How will my clinician measure my follicle growth?
Your RE will use a transvaginal ultrasound to monitor your follicular sizes throughout the ovarian stimulation process of IVF treatment. During these ultrasounds, they will locate, count, and measure your follicles. It’s normal for the number of follicles to change slightly throughout your ovarian stimulation process.
Combined with your blood work, your RE can continue to tailor your medications to ensure that you are developing the optimum number of follicles for your ovaries in a way that’s safe for your body. Because of this, there is no “standard” ovarian stimulation protocol that your RE will follow; they will choose medications, dosages, and a schedule that will optimize the number of eggs they can retrieve.
(Want to learn about the ways that clinics can use AI tools, like the ones we build here at Alife, to optimize your ovarian stimulation outcomes? Click here!)
Should I track my follicle growth?
Tracking your follicular growth can help you better understand what is happening in your body, set expectations for your IVF outcomes, and empower you to ask questions of your doctor so you can participate actively in your care. To track your follicle growth (and other IVF results) with ease, check out the Alife Health mobile app today!
Recent Articles
References
-
Tavaniotou, A., Albano, C., Smitz, J., & Devroey, P. (2002). Impact of ovarian stimulation on corpus luteum function and embryonic implantation. Journal of Reproductive Immunology, 55(1-2), 123–130. https://doi.org/10.1016/s0165-0378(01)00134-6
-
Baerwald, A. R., Walker, R. A., & Pierson, R. A. (2009). Growth rates of ovarian follicles during natural menstrual cycles, oral contraception cycles, and ovarian stimulation cycles. Fertility and Sterility, 91(2), 440–449. https://doi.org/10.1016/j.fertnstert.2007.11.054
-
ROSEN, M., SHEN, S., DOBSON, A., RINAUDO, P., MCCULLOCH, C., & CEDARS, M. (2008). A quantitative assessment of follicle size on oocyte developmental competence. Fertility and Sterility, 90(3), 684–690. https://doi.org/10.1016/j.fertnstert.2007.02.011
Images:
Fanton, M., Nutting, V., Solano, F., Maeder-York, P., Hariton, E., Barash, O., Weckstein, L., Sakkas, D., Copperman, A. B., & Loewke, K. (2022). An interpretable machine learning model for predicting the optimal day of trigger during ovarian stimulation. Fertility and Sterility, 118(1), 101–108. https://doi.org/10.1016/j.fertnstert.2022.04.003
Share this
Recent Articles
Learn everything you need to know about IVF
Join the newsletter for IVF education, updates on new research, and early access to Alife products.



